World Covid-19 tracker: Latest cases and deaths by country (cnn.com)
A LIFE RESET: What Do I mean by You Are The Answer”?
I mean you have to help yourself, no one can do it for you. God will help you but you have to do your part.
God helps those who help themselves.
A couple weeks ago I came down with Corvid 19 and my life hasn’t been much fun since.
In just a few miles of driving I went from feeling myself to having a really warm body and being disoriented. We were having heavy rain as I slid through a rural intersection and glanced off a road sign as the road name sign came down but neither damaged the sign or my car. Thank GoD. Luckily a young man of 22 was following me and told me you look really sick and told me to go back home and he would report to the local
cops what happened.
When I returned home, which was about a 5 mile drive. I parked my car in the driveway and hurried into the house. It was diaherra. After All that I scuffled back out to my car for the next two weeks. As I went into the house I passed out for the next few days only getting up to go to the bathroom. As I noticed my first trip back
I noticed my legs were knotted and could barely walk without the usage of my cane from a prior year knee injury.
The next three days I found myself drinking Schweppes Tonic Water began in 1783 as the world’s original
soft drink. Its founder, Jacob Schweppe, was drawn to the new art of carbonating beverages, so he refined and patented his own process of creating mineral water. Customers referred to Schweppes as
LIGHTNING IN A BOTTLE because it was the first bottle of its kind to retain carbonation.
How Much Tonic Water Must You Drink to Ease Leg Cramps? – YouTube
While in combination Nature’s Sunshine Zinc provides 166 percent, or 25 mg, of the daily value of this important trace mineral. Found in large amounts in the bone and muscle, zinc is one of the body’s most abundant minerals. Zinc supports a healthy immune system, helps metabolize sugar, assists in forming DNA, and encourages energy production as well as helping metabolize protein. Nature’s Sunshine Zinc is blended with an herbal base of kelp plant, alfalfa herb, and thyme herb.
Throughout my ordeal from day one. I have been using mouthwash to get that unhealthy metal taste out of my mouth. Figuring it may cause an unhealthy buildup in my belly. All the while not hungry I ate Oikos Greek Yogurt has 87 Calories and 8.00 g of Protein per 100 gram serving according to the nutrition facts provided by the USDA Food Composition Database. Calories, Carbs and Protein.
One serving of nonfat Oikos Greek Yogurt …
I was eating Oikos Organic Triple Zero Mixed Berry Nonfat Greek Yogurt, 5.3 Ounce — 12 per case.
And eating Chicken Noodle Soup or Frosted Mini Wheats to keep my bowels moving.
I ate a lot of Sherbet ice cream which helped coat my dry throat and further reduce my fever from Prairie Farms Dairy. Which is a dairy cooperative founded in Carlinville, Illinois, and headquartered 35 miles to the south in Edwardsville, Illinois, a suburb within Greater St. Louis. As a dairy cooperative, Prairie Farms receives milk from producers and converts it into many different products, including cheese, butter, ice cream, sour cream, cottage cheese, various dips, yogurt, and fluid milk. Prairie Farms Old Fashioned Rainbow Sherbet Orange, Raspberry, Lime; Prairie Farms Old Fashioned Rainbow Sherbet Orange, Raspberry, Lime 4 quart.
Drinking Alka65 Purified #Water test – pH and TDS – YouTube was key to keep my throat wet and urine flowing as well. It was important because the more dehydrated I became the harder it was for me to breathe (Traditional Medicinal Breathe Easy Tea was a big key and Seagate Olive Leaf Mint Tea.) While Chamomile is a very soothing, slightly sedative herb and helps calm the stress that comes with this kind of cough and difficulty breathing. Safety Factor: Chamomile is considered a very safe herb. However, like Echinacea, some people may experience an allergic reaction to Chamomile.
Today I struggle back with SHORTNESS OF BREATH, swollen feet and legs because of the
Acetaminophen PM Caplets – and NyQuil™ which helped. But for me it may have been an allergic reaction. Unkers Therapeutic Rub for Joint Pain, Sore Muscles, Burn Cream, or Calm Your Cough 13.5 ounces. Unkers medicated SALVE is very effective pain relief cream. HIGH QUALITY pure essentials oils (camphor oil, eucalyptus, menthol crystals and more) are used to formulate this Unkers salve. Unkers deep penetrating pain relief is PETROLEUM BASED. First aid salves for pain relief are made in the USA.
MULTI-PURPOSE salve for pain can be used for joint & muscle soreness, skin irritation, cough, minor burns, muscle sprains, sore throat, etc. rubbing it on the soles of your feet may be most effective.
BUT I AM GETTING BACK TO NORMAL Eating ELDERBERRIES.
Spinach, Asparagus, Sauerkraut and eating baked potatoes.
My feet getting back to normal size with a cup of vingar and
a pack of Johnson Foot Soap in a foot basin for 20 minutes!
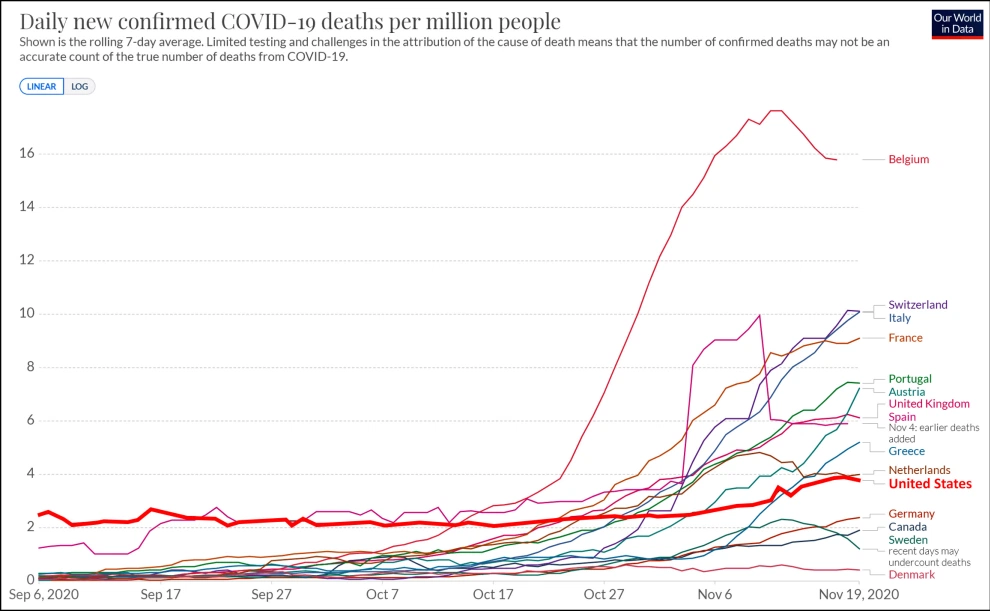
After the first cases of Covid-19 were confirmed in the United States on January 20, it took almost 100 days to reach 1 million infections. Now, the country has added more than 1 million cases to its grim total in just five days. From Tuesday to Saturday, 1,000,882 new coronavirus cases were reported in the US, according to data from Johns Hopkins University, bringing the totals to more than 14.5 million confirmed cases and 281,199 deaths from the virus. November registered frightening peaks in the daily number of coronavirus cases — reaching 100,000 for the first time, as well as spikes in hospitalizations and deaths. On the second day of December, more than 200,000 new cases were reported for the previous 24 hours. As the impacts of Thanksgiving travel and gatherings begin to reveal themselves, and hospitals fill to capacity,
experts say it is likely going to get only worse.
“Every single day, thousands more people are getting this virus, and we know that means that in a few days,
in a week, hundreds of people are going to be coming to the hospital and hundreds of people are going to die,” Dr. Shirlee Xie, associate director of hospital medicine for Hennepin Healthcare in Minneapolis, told CNN,
her voice breaking with emotion.
“I think that sometimes when you hear statistics like that, you become numb to what those numbers mean,”
she said. “But for us, the people that are taking care of these patients, every single number is somebody we have to look at and say, ‘I’m sorry, there’s nothing more I can do for you.'” More than 100,000 Covid-19 patients have been hospitalized nationwide for the past four days, according to the Covid Tracking Project.
Millions of Californians face stay-at-home orders.
In the last week, hospitalizations in Los Angeles County have tripled, and the number of available hospital beds in the area could dwindle to none in two to four weeks if cases continue to climb, Los Angeles Mayor Eric Garcetti said Friday. In response to the growing threat, the Southern California region will be under a new stay-at-home order beginning at 11:59 p.m. Sunday. The order will apply to Los Angeles, San Diego, Orange, Riverside and San Bernardino counties. The San Joaquin Valley also will be under stay-at-home orders at that time, local officials announced Saturday, after the region’s intensive-care-unit capacity fell below 15%. More than 4 million people live in the region. On Friday, officials in the San Francisco Bay Area issued a stay-at-home order, restricting the activities of more than 5.8 million people. It affects the counties of Alameda,
Contra Costa, Marin, Santa Clara and San Francisco, as well as the city of Berkeley.
While the Bay Area has not met the threshold of less than 15% capacity, officials warn they’re seeing evidence of transmission over Thanksgiving weekend that could fuel a surge. “I don’t think we can wait for the state’s new restrictions to go into effect later this month,” Contra Costa Health Director Chris Farnitano said Friday.
“We must act swiftly to save as many lives as we can. This is an emergency.”
“It really is time for us to pull back on the activity and see if we can turn this thing around before hospitals get overwhelmed,” said Dr. Robert Wachter, chairman of the department of medicine at University of California, San Francisco, pointing out that California has had a “better than average performance” throughout the pandemic.
“I see other parts of the country that are still open, even though the case rates and hospitalization rates are far worse than here,” he said. “So, I think we’re acting correctly.”
Adults must get vaccinated for students to return to school.
It will likely be months before all adults in the US can be vaccinated against the virus, and the wait will be even longer for children — but they can still be protected by vaccine distribution, Wachter said. “I think it’s reasonable to expect that the kids will be back in school in the fall, not so much because all of them have been vaccinated — although I hope they will — but everybody around them has been vaccinated, and the rate of virus in their communities has fallen to a point that is perfectly safe for them to be in school,” Wachter said.
Earlier this week, vaccine advisers to the US Centers for Disease Control and Prevention voted 13-1 to recommend that both health care workers and residents of long-term care facilities be first in line for any vaccines that get the green light from the US Food and Drug Administration. Moncef Slaoui, chief scientific adviser for the public-private vaccine program known as Operation Warp Speed, said he hopes to see a “quite significant” drop in coronavirus illness and death among the elderly population by January’s end.
Noting that 40% to 50% of US deaths are coming from elderly Americans residing in nursing homes or long term care facilities, Slaoui told CNN, “We should be able to have immunized that full population, and the healthcare workers that take care of them by the end of the month of December or by the middle of the month of January.”
By the middle of March, he added, the United States should have vaccinated its highly susceptible population, which is about 100 million people, while the rest of the country “will not all have the vaccine in our arms before May or June.” The vaccine, which will come in two doses — a challenge to produce and distribute in the necessary quantities — will likely reach healthy, non-elderly Americans with no known underlying health conditions in late March to early April, said Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases.
Kids are likely to be vaccinated relatively late in the game because Covid-19 vaccines are largely untested on children. The National Vaccine Advisory Committee voted Friday not to recommend emergency use of a Covid-19 vaccine in children, noting that children generally experience a milder version of the disease. Wachter says that if adults get vaccinated, children could reap the benefits. “If we can get everybody else vaccinated — we can get all the adults vaccinated and get the virus to die out because we get somewhere near herd immunity — the kids may be less important.”
People can catch COVID-19 twice. That’s the emerging consensus among health experts who are learning more about the possibility that those who’ve recovered from the coronavirus can get it again. So far, the phenomenon doesn’t appear to be widespread—with a few hundred reinfection cases reported worldwide—yet those numbers are likely to expand as the pandemic continues.
Fact Check: Do You Need a COVID-19 Vaccine If You Already Have Had the Virus? (msn.com)
Not only does it take a while for subsequent bouts to show up, health departments must make sure that alleged cases really are reinfections because coronavirus residue can linger for weeks. For example, University of Alabama football coach Nick Saban made headlines
just before Thanksgiving when he tested positive for a second time. But it is unclear if he was truly re-infected because of a blind spot in how officials screened for cases during his first episode back in October.
Because COVID-19 reinfections are still relatively rare,
they can’t be blamed for the ongoing surges. Still, these incidents could be unwelcome news for coronavirus veterans who have been hoping their experience might have given them a so-called immunity passport. Such accounts show that recovering from the SARS-CoV2 coronavirus isn’t an excuse to shed masks and flout social-distancing rules while the pandemic is in full swing. In October, an 89-year-old Dutch woman was the first documented death of someone who had contracted the coronavirus a second time.
Immunity may wane over time—just like it does with other kinds of coronaviruses—and getting sick may even prime some people to suffer worse symptoms if they catch the virus a second time. Take this case study, published in October in The Lancet: In early April, a 25-year-old Nevada man showed up to a community testing center complaining of a sore throat, cough, headache, and nausea. Sure enough, he tested positive for COVID-19, and he went home to isolate. In the weeks that followed, two more tests confirmed he had fully recovered.
Yet by the end of May, the coronavirus had struck again. This time, he came down with an even worse case that was marked by shortness of breath and required him to go to the emergency room for oxygen.. Other countries have also reported reinfection rates that suggest the true global toll is unknown but potentially dangerous.
Last month, Sweden launched an investigation into 150 cases. In Brazil, scientists are tracking 95 cases. And Mexico claimed to have 258 reinfection cases as of mid-October—nearly 15 percent
of which were severe, and 4 percent were fatal. The nation’s datasets show that people who suffered from serious first cases were more likely to be hospitalized with subsequent infections. “The takeaway is that reinfection is certainly possible,” says Richard Tillett, a biostatistician at the Nevada Institute of Personalized Medicine at the University of Nevada, Las Vegas, and lead author of the case study.
“It seems uncommon and maybe even rare.
But it’s real and can happen.” ”Why spotting reinfection is harder Reinfections are hard to document because researchers can’t simply rely on patients’ accounts of return symptoms or on routine COVID-19 tests involving polymerase chain reaction (PCR). They need stronger genetic proof, which calls for different technologies.
A new mutation appears in SARS-CoV-2 every 15 days, on average.
So far, those natural changes are not so extensive that they alter the nature or potency of the coronavirus,
a.k.a. it isn’t a new strain. But they can provide evidence that the patient’s second bout wasn’t the same as the original infection.
“It’s not that patients get re-infected from a new strain,” says Nathan Grubaugh, assistant professor of epidemiology at Yale School of Public Health in New Haven, Connecticut. Such sequencing data, he says, simply offers a “genetic signature” to show if the recurrence of the disease stems from a new infection. That’s how the Nevada team was convinced that their patient didn’t simply suffer from a persistent, clandestine infection that suddenly had grown worse. “Our argument is that he caught it from a second source because we observed six different mutations,” says Tillett. Using the combination of patient histories and genetic sequencing is the bona fide way to track reinfections; they can’t be gleaned by surges measured with standard testing. To do this going forward, health labs will need to unify their practices and store specimens for the long term.
A recent survey in Qatar identified 243 potential reinfections based on case history, but only four had enough genetic material to be confirmed.
This need prompted the U.S. Centers for Disease Control and Prevention in late October to establish new “gold standard” guidelines. (Saban’s first case happened before this guidance arrived.) Local health officials who learn of alleged repeat cases are now encouraged to send specimens to a testing lab that is equipped with genetic sequencing capacity, as well as to carefully document symptoms and the interval between initial infection and a suspected re-infection.
That time interval is particularly critical because it could help answer the question:
How long will our immunity last against SARS-CoV-2?A kinder COVID-19 the second time around?
Much of society’s return to normalcy hinges on the duration and strength of our COVID-19 immunity. Along with determining how people recover from the disease, it will dictate how often a vaccine needs to be taken to control the pandemic, and even whether social distancing will endure.
But it takes time to prove if immunity to any disease is durable. For early clues to how
COVID-19 might behave, health experts tried to divine the risk of reinfection by looking at other human coronaviruses. For example, one study of four seasonal coronaviruses published in September in Nature Medicine found that reinfections could occur as soon as six or nine months later, but were more likely to be observed at 12 months. But a body’s response to SARS-CoV-2 is unlike that of seasonal viruses because humans and those latter germs have had time to adapt to each other.
Grubaugh generally attributes the phenomenon of waning immunity to patients’ lack of antibodies for a particular virus. These proteins are produced in the immune system in response to an infection. They help stifle the germ as it invades and are widely believed to ward off future attacks. Evidence suggests that 95 percent of people produce antibodies two weeks after the COVID-19’s onset. Grubaugh says it’s possible SARS-CoV-2 antibodies could fade over time and you could become susceptible again, but he doesn’t expect that to happen for years or decades. More likely is that some people don’t develop a foolproof antibody response
in the first place, he says.
The latter appears to be what happened to a 33-year-old Hong Kong man who was first sick in March and then developed an asymptomatic case in August. Even though he didn’t exhibit the classic cough, fever, or headache the second time, he still became a potential spreader. Grubaugh suspects most reinfections at the moment are due to a person’s immune system being compromised. What makes the reinfection story even more mystifying is that such accounts come at a time when emerging research suggests immunity to COVID-19 might actually be robust. Some preliminary studies do show that antibody levels drop within a couple months after SARS-CoV-2 infections, but others argue that these waning numbers don’t mean a loss of protection.
The immunity symphony
In fact, fading antibodies may be a sign of a normal and healthy immune response. In November,
a British study published as a preprint (meaning that it was not peer reviewed) reported that an initial flood of antibodies soon after infection corresponded with protection for six months—even if the antibody levels faded over time. The study documented only three asymptomatic reinfections among 1,246 health-care workers who had detectable antibodies early on.
That’s because antibody levels don’t reveal the full story of a person’s ability to fight off future infections,
says S. Vincent Rajkumar, an oncologist and professor of medicine at the Mayo Clinic in Rochester, Minnesota, who studies immunity.
Think of the human immune system as an orchestra, and among its versatile players are
B cells and T cells. When SARS-CoV-2 invades, the body’s opening movement is frantic.
Some B cells rev up swiftly, producing that first burst of antibodies within a week or two. Simultaneously, a group of T cells—known as killers—hunts down any other cell infected by the coronavirus and gets it to self-destruct. A separate type of T cell—known as helpers—guides both of these crisis responses. If any part loses the harmony, it can throw off the entire production and actually cause more damage rather than less.
While all of this is happening, the immune system is also learning.
A fraction of these B cells and T cells get stored away as so-called memory cells.
After recovery, the memory cells continue to work behind the scenes to prevent reinfections.
“The cells that made those antibodies will still be around. It will be difficult for a new infection to cause the same amount of harm as the first one. The body already knows how to respond,” Rajkumar says.
This is why scientists were excited in July when a research paper showed that memory T cells were still detectable years after people recovered from the 2002-2003 SARS coronavirus,
a close cousin of this year’s plague.
Now, the latest evidence suggests that both B cells and T cells generated from COVID-19 infections are
also likely to stick around for the long run. One preprint, published November 16, began to sketch out the lifespans for these critical components of the immune system among 185 coronavirus patients. It showed that memory B cells remained widely abundant after six months, while memory T cells had been reduced, but only by half. Another study from November found that a hundred health-care workers who contracted the coronavirus in the spring and showed mild or few symptoms—and didn’t produce many antibodies to begin with—still had robust T cells six months later.
What’s unknown is how these B cells and T cells will act if the body is re-exposed to the coronavirus.
Will they produce an inflammatory response that somehow leads to a worse case later with more severe symptoms? Or will they blunt the outcome and yield the mild reinfections witnessed in some early reports?
If the trajectories of cold-causing coronaviruses are any reassurance, getting COVID-19 again won’t be nearly as miserable the second time for most people, says Rajkumar. That means the Hong Kong case would be the norm, while the Nevada man who developed a more severe case after being re-infected might not be typical. For now, there isn’t enough long-term research to know if B cells and T cells activated by the cutting-edge mRNA vaccines on the verge of approval will offer lasting protection, though a recent, two-month study in mice suggests that the answer could be “yes.” In the meantime, even if recovered COVID-19 patients are counting on a less painful second episode, they shouldn’t toss aside their masks. They could still catch the virus and pass it to others, who might then become sick. “You might get re-infected, and your symptoms might be so mild that you don’t know about it,” says Rajkumar, adding that mask-wearing should continue until the world has reached herd immunity. “It’s wise to wear a mask even if you’ve had COVID-19 out of concern for others.” Israeli-made mask eliminates over 99% of coronavirus, lab tests suggest – The Jerusalem Post (jpost.com)
