But there is a new dementia story being told. It is a story of joy and growth.
It is a story being told by people living with dementia, for people living with dementia, who want to disrupt the status quo and tell you that they are still here and their lives have meaning. Across the country people living with dementia and friends are creating opportunities to socialize and reconnect
with their communities through Alzheimer’s Cafes, art and fitness classes, theater and museum outings.
Advocates and researchers are discovering untapped potential for music and arts to engage people considered lost to dementia, as demonstrated in the groundbreaking documentary film Alive Inside that debuted nationally through Dr. Thomas’ first national tour in 2014.
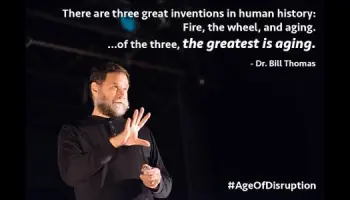
Dr. Bill Thomas will partner again with Alive Inside director Michael Rossatto-Bennett to invite communities to “Disrupt Dementia” and experience a new vision of intergenerational engagement and transformation through the power of music and memory. Watch Alive Inside (2014) – Free Movies | (tubitv.com) .
Disrupt Dementia documentary film by Rossato-Bennett
Disrupt Dementia is a two-part afternoon workshop that will premiere a new documentary film by Rossato-Bennett, followed by live music from Nate Silas Richardson and international recording artist Samite. The second half of the workshop is currently in the design stage — the process will be iterative and we’re working with Jennifer Carson, Ph.D., a pioneer in the field of authentic partnership research, and Kyrié Carpenter, M.A., anti-ageism activist and counselor, to give voice to and empower people living with cognitive change.
“Inspiring people to disrupt dementia can have a ripple effect in helping them to disrupt aging both personally and in their communities,” Dr. Thomas said. “Disrupting people’s deepest and most ageist fears will change how they feel about their own aging.” Dementia: the Joy of Living an Improvisational Life.
Many recognize the value of improvisation in supporting everyone to live with (perform) dementia in new and more joyful ways.
by, Mary Fridley
In her December 2017 post, “Stealing Hope,”
Anne D. Basting passionately challenges the fear and stigma-inducing “tragedy narrative” that distorts how people living with dementia are seen within the broader culture. The two of us were especially inspired by Anne’s closing words, “Family members and friends…can learn to shift toward creativity to find emotional connection, to play, to create new moments and experiences together.”
They really resonated, you see, because we are two “developmentalists” who believe that play and performance are key to how human beings continue to grow and develop regardless of age, life circumstance and/or cognitive and physical ability, In fact, we are leading a workshop series, “The Joy of Dementia (You Gotta Be Kidding)” in cities across the country.
We are far from alone.
Across the globe, practitioners, caregivers and patients are embracing play, performance and the arts. Many recognize the value of improvisation in supporting everyone to live with (perform) dementia in new and more joyful ways. As actor and improviser Karen Stobbe has written, “Flexibility, adaptability, courage, spontaneity, listening, generosity, acceptance…are characteristics of an excellent caregiver. They are also qualities of an excellent improvisational performer.”
Improvisation, along with other creative approaches that reawaken connection and joy, are serious challenges to the underlying concepts (individual self, identity, memory, etc.) that shape our understanding of what it means to be human. Rightly or wrongly, in Western culture, it’s primarily our cognitive functioning that is thought to make us human. And this is what people with dementia lose – our ability to think, to reason, to recognize, to remember, to know. We must ask, does our society believe that they have lost what makes them human? Sadly, this is precisely how people living with dementia are too often related to – as people no longer expect to learn and develop, adapt and connect – an expectation as devastating as the loss of memory.
But what if this belief has severely limited our capacity to appreciate the multitude of other ways (creative, physical, poetic, silly) human beings can and do connect all the time? And what if these other ways of relating enable us to deal with the dementia experience – not to mention the increasingly uncertain world in which we are living – with compassion, creativity and growth?
“Development lens” on dementia – Bing video
These are just some of the questions we have been asking over the last five years as we focus a “development lens” on dementia – a journey made more poignant when Susan’s sister was diagnosed with Alzheimer’s and Mary’s mother passed away from dementia-related complications.
As each of us slowly transformed our relationships with these dear family members, we realized we were drawing on the universal capacity to play, create and connect with those who do not have adult cognitive functioning. We mean babies! Think of how they learn to speak. They babble – they “say” “ga ga goo goo, ba de ba” and adults around them say, “I don’t like broccoli either, but it’s good for you.” Far from treating their babble as nonsense, adults naturally (it seems) take that babble and use it to play “having a conversation,” encouraging babies to play, pretend, imitate and imagine to their heart’s content.
When adults, especially those with cognitive limitations, “babble,” it can be very difficult to see or hear them as offerings to create with. Mostly, their sounds get interpreted (“Mom is crying, so she must mean she is in pain”), or reacted to with anger, frustration and/or great sadness. Rarely are they the source of improvising a conversation or a scene together.
What would it mean to bring this new way of being and seeing to our relationships?
To respond in a way that encourages the joy of discovery and the emergence of creativity?
To embrace the risk-taking and dream-making that is possible when improvisational play is how we do everything in our lives?
Living with dementia will affect a person’s feelings, thoughts and responses.
It is important to recognize and respond to the person’s emotional needs.
1. Understanding and supporting a person with dementia | Alzheimer’s Society (alzheimers.org.uk)
2. The practical impact of dementia | Alzheimer’s Society (alzheimers.org.uk)
3. You are here: The psychological and emotional impact of dementia
4. Coping with dementia | Alzheimer’s Society (alzheimers.org.uk)
5. Carer’s: looking after yourself when supporting someone with dementia | Alzheimer’s Society (alzheimers.org.uk)
6. Understanding and supporting a person with dementia – useful resources | Alzheimer’s Society (alzheimers.org.uk)
The psychological and emotional impact of dementia.
Reactions to diagnosis.
A diagnosis of dementia can have a huge impact on a person’s life. Someone recently diagnosed with dementia is likely to experience a range of emotions. These may include grief, loss, anger, shock, fear, disbelief and even relief.
Some people may struggle to deal with these emotions and they may move between emotions as they adjust. They may feel afraid about the future, scared about moments of confusion and forgetfulness, and upset about the impact dementia has on those around them.
The confirmation of a diagnosis may trigger depression and anxiety in some people. There are a number of talking therapies and – if needed – drug treatments available for depression and anxiety. Lifestyle changes can help too.
Those around the person will also have their own emotional reactions to cope with. It is important that both the person with dementia and the people around them feel able to, and are encouraged to, express their feelings.
Some people experience positive reactions when they receive a diagnosis of dementia. They may be relieved to know what is wrong or be glad to be able to plan ahead. Some may use the experience to re-evaluate their situation and focus on the activities and relationships that make them happy.
Supporting the person’s emotional responses: tips for carer’s
Try to understand how the person with dementia feels & thinks.
Do not dismiss a person’s worries – listen and show them that you are there for them.
Try to enjoy the moment and try not to spend too much time thinking about what the future may or may not hold.
A sense of humor may help, if the time feels right.
Music Therapy New Order – Blue Monday – YouTube
I love how people in the 80’s made this so it can sound more futuristic, but instead now when we hear stuff like this, we feel nostalgic and think of the 80’s. Now you hear it and you feel nostalgic, but literally everything in the 80’s looks like they tried to make everything look futuristic, but instead ended up just being nostalgic designs from the 80’s. All the neon bright colors? And for this song, it had many different sound effects that some people will now think of the 80’s when they hear.
Look up “The 30 year cycle” or how culture recycles itself every 30 years. In the 2010’s we were nostalgic for the 80’s. In the 80’s people were nostalgic for the 50’s. In 2040: people will be nostalgic for the 2010’s. People in 1980: This makes me want to be in the 2020’s.
People in 2020: This makes me want to go back to the 80’s

Bohemian Rhapsody is the oldest song in history to ever pass 1.4 billion streams on Youtube. Queen – Bohemian Rhapsody (Official Video Remastered) – YouTube
Emotions and feelings.
People with dementia often experience changes in their emotional responses. They may have less control over their feelings and how they express them. For example, someone may be irritable, or prone to rapid mood changes or overreacting to things. They may also appear unusually uninterested in things or distant.
These changes are often difficult for carer’s to deal with. It can help if carer’s remember that they are partly caused by damage to the person’s brain. Someone may react more emotionally to a situation than might be expected (e.g. by becoming tearful or agitated) because some of their factual memories or ability to think clearly about the situation have declined. It is important to look beyond the words or behavior’s you can see to the feelings that the person might be trying to express. Strong emotions may also be caused by unmet needs. Carers should try to work out what these needs are and meet them where possible.
Confidence and self-esteem.
Dementia may cause people to feel insecure and lose confidence in themselves and their abilities. They may feel they are no longer in control and may not trust their own judgment. They may also experience the effects of stigma and social ‘demotion’ – not being treated the same way by people – as a result of their diagnosis. All of this can have a negative impact on the person’s self-esteem.
Dementia may also have an indirect effect on someone’s self-esteem by affecting other areas of a person’s life. Health issues, financial circumstances, employment status and, importantly, relationships with those around them may suffer.
Some people, however, form new relationships as a result of their diagnosis, through activities such as attending a class or a support group. High self-esteem allows some people to cope better with chronic health conditions.
Supporting the person with dementia to maintain self-esteem: tips for carers
Offer the person plenty of praise and encouragement – celebrate successes and focus on positives.
Avoid harsh criticism or belittling comments.
Ensure people have time to do the activities they enjoy and that give them purpose.
If a person makes a mistake, try to be as supportive as possible.
Help people to maintain existing social relationships and form new ones.
This can be done by facilitating joint activities with friends and family, joining hobby groups and encouraging conversation.
Dr.Dale Bredesen’s is known for his work in translating his scientific research into effective treatments for Alzheimer’s disease. He is the author of the book The End of Alzheimer’s and the ReCODE protocol – reversal of cognitive decline/
Dementia Reimagined: Building a Life of Joy and Dignity from Beginning to End. Now in paperback, the cultural and medical history of dementia and Alzheimer’s disease by a leading psychiatrist and bioethicist who urges us to turn our focus from cure to care. Despite being a physician and a bioethicist, Tia Powell wasn’t prepared to address the challenges she faced when her grandmother, and then her mother, were diagnosed with dementia–not to mention confronting the hard truth that her own odds aren’t great.
In the U.S., 10,000 baby boomers turn 65 every day; by the time a person reaches 85, their chances of having dementia approach 50 percent. And the truth is, there is no cure, and none coming soon, despite the perpetual promises by pharmaceutical companies that they are just one more expensive study away from a pill.
Dr. Powell’s goal is to move the conversation away from an exclusive focus on cure to a genuine appreciation of care–what we can do for those who have dementia, and how to keep life meaningful and even joyful. Reimagining Dementia is a moving combination of medicine and memoir, peeling back the untold history of dementia, from the story of Solomon Fuller, a black doctor whose research at the turn of the twentieth century anticipated important aspects of what we know about dementia today, to what has been gained and lost with the recent bonanza of funding for Alzheimer’s at the expense of other forms of the disease. In demystifying dementia, Dr. Powell helps us understand it with clearer eyes, from the point of view of both physician and caregiver. Ultimately, she wants us all to know that dementia is not only about loss–
it’s about the preservation of dignity and hope. Tia: 9780735210905: Amazon.com: Books

Our Elderflowers visit people living with dementia in hospitals,
hospices and residential care homes. These are ladies and gentlemen with full and rich lives behind them who now often feel isolated, confused and frightened, and struggle with the complexities of the present day.
Elderflowers help people living with dementia to: improve emotional regulation counteract feelings of frustration, isolation and boredom improve their social and personal interactions reduce sedentary behavior’s address sensory decline enhance agency and self-efficacy.
A ‘made to measure’ approach
Each intervention is ‘made to measure’ and improvised. Empathy, authenticity and playfulness sit at the heart of our approach and while interventions might involve music, singing, magic, mime or gentle slapstick, we always put the individual’s needs first. The Elderflowers – joy and laughter for ladies and gents living with dementia
“I hope you make everyone as happy as you made me today. You are wonderful!” Hearts and Minds – Elderflowers – Bing video
What is Music Therapy? – Bing videoIn Dementia Units (hearts minds.org.uk)
Sophie Rocks Harp – Bing video
HeartsMindsUK – YouTube
Exiting the matrix  questioning everything
questioning everything 
Govt. does not dictate my health decisions Liberals are now societies’ conformists:
Think this page could be useful to someone?
Anxiety – Fear – Change in Light – Pain – Stress – Surprises and Dementia
Living with Dementia – Creating Moments of Joy – YouTube
What Emotions Affect Alzheimer’s – Bing
Dementia: the Joy of Living – Bing video
Dementia Joy of Living – Bing video
Inside Dementia Minds – Bing video
