What Is It, Causes, and More
Author: Corinne Tarantino, MPH
Editors: Alyssa Haag, Kelsey LaFayette, BAN, RN
Illustrator: Jillian Dunbar
Copyeditor: Joy Mapes
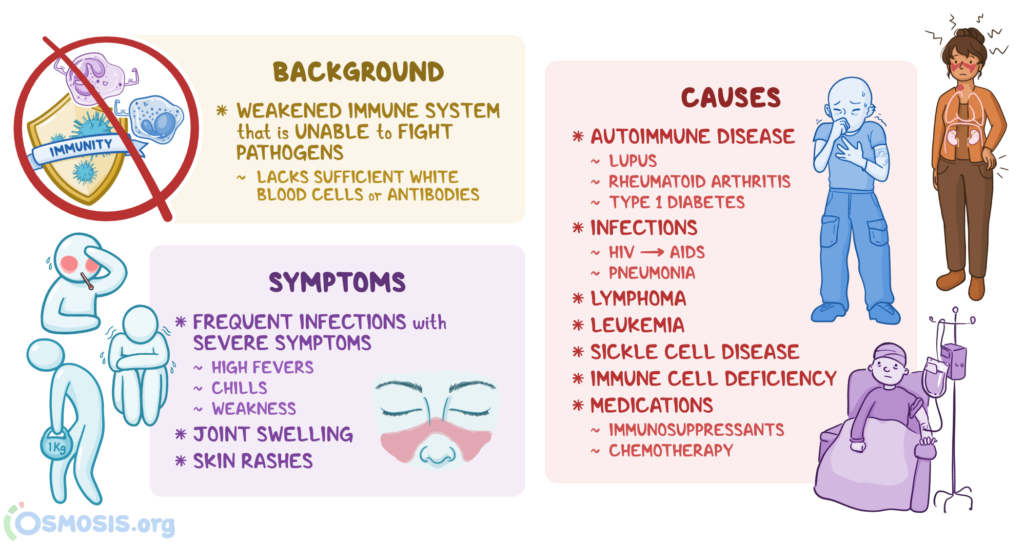
What is a suppressed immune system?
The immune system consists of the body’s defenses against most foreign bodies (i.e., pathogens), and it includes white blood cells, antibodies, organs (e.g., the lymphatic
organ system, spleen, thymus) and other parts of the body. When a body lacks sufficient
white blood cells or antibodies, the immune system is considered suppressed.
A suppressed immune system is weakened to the point that it cannot mount a proper immune response to protect the body from pathogens, such as bacteria, viruses, and other infectious microorganisms. Therefore, people with a suppressed immune system become vulnerable to various infectious diseases.
What causes immune suppression?

There are many different causes of immunosuppression, including diseases,
medications, and lifestyle factors. Most commonly, a suppressed immune system can
be caused by an autoimmune disease, in which the immune system attacks its own cells.
This occurs when the immune system produces self-targeting antibodies, which cannot distinguish between self and non-self and will therefore mistakenly attack an individual’s own body. Some of the most common autoimmune diseases include systemic lupus erythematosus, rheumatoid arthritis, and type 1 diabetes.
Both systemic lupus erythematosus and rheumatoid arthritis are characterized by inflammation or swelling of the joints, while type 1 diabetes is characterized by impaired release of the insulin, a naturally occurring hormone that regulates blood sugar levels, from the pancreas.
There are various viral and bacterial infections that can also suppress the immune response. The most common example of long-term viral immunosuppression is the
human immunodeficiency virus (HIV), which can develop into acquired immune deficiency syndrome (AIDS). HIV infects and destroys CD4+ T cells, a major group of white blood cells involved in responding to viral pathogens. This leaves the immune system suppressed and vulnerable to other infections. Pneumonia is another example. Often the result of a bacterial infection (e.g., Staphylococcus aureus or Streptococcus pneumoniae), pneumonia causes inflammation of the lungs.
The damage pneumonia can do to the lungs can suppress the immune system and
increase the risk of future infections. Other diseases — including lymphoma, leukemia, and sickle cell disease — may also suppress the immune system, as they can affect the spleen, an important organ involved in the immune response.
Lymphoma and leukemia are types of cancer that can cause a buildup of lymphoma cells, red blood cells, and platelets in the spleen. This buildup can also make the spleen swell and work less efficiently, which may eventually lead to splenic dysfunction. In the case of sickle cell disease, the characteristic sickle-shaped red blood cells can block the spleen’s blood vessels, causing swelling and impairing the spleen’s functioning.
Rarely, an individual may be born with poor development or functioning
of one or more immune cell types, called a primary immune deficiency.
These conditions typically affect the four main types of antibodies:
IgA, IgE, IgG, and IgM. Each type of antibody plays various roles in fighting off pathogens.
The most common types of primary immunodeficiencies include selective IgA deficiency
(i.e., deficiency in the IgA antibody), X-linked agammaglobulinemia (i.e., deficiency in all
classes of antibodies), and hyper-IgM syndrome (i.e., deficiency in IgA, IgE, IgG antibodies).
Moreover, there are several medications that can weaken the immune system.
Immunosuppressants are a class of medications that are prescribed intentionally to
suppress the immune system, such as to treat an autoimmune disease or prevent the
body from rejecting an organ transplant. Immunosuppression can be a side effect
of some treatments, like chemotherapy.
Prescribed to destroy cancer cells,
Chemotherapy medications often suppress the immune system at the time of treatment and for a few months following the conclusion of treatment. Occasionally, lifestyle factors, such as long-term alcohol misuse and severe malnutrition, may also result in a weakened immune system.
What are the signs and symptoms of a suppressed immune system?
Signs and symptoms of a suppressed immune system include frequent infections accompanied by severe constitutional symptoms, such as high fevers, chills, and weakness. Also, if an individual requires many antibiotic treatment courses in one year, this may be indicative of an underlying immune response concern.
Specifically, the American Academy of Allergy, Asthma & Immunology suggests that if a child needs more than four antibiotic courses in a year, or an adult needs more than two,
a healthcare professional should assess for underlying immune suppression.
For both children and adults, having pneumonia twice in a lifetime, needing preventative antibiotics, or having chronic sinus infections may also indicate a suppressed immune system.
Depending on the cause of the immunosuppression, there may be additional symptoms, such as feeling tired and weak or experiencing body aches and pains. Some autoimmune diseases may present with swelling around the joints and rashes on the skin. For example, people with lupus tend to have a distinctive “butterfly” rash across both cheeks; however, unlike rashes caused by an allergic reaction, it is usually not an itchy rash.
How is a suppressed immune system diagnosed?
Diagnosis often begins with a medical examination, during which a clinician asks
for the individual’s past medical and family history, assesses their signs and symptoms, and performs a physical exam. If immunosuppression is suspected, blood tests will often be performed, particularly a complete blood count (CBC).
A CBC will measure how many white blood cells an individual has, and it can provide additional information that may help to identify what part of the individual’s immune system is suppressed. Additional blood tests may be performed depending on the suspected cause. In some cases, imaging, such as an X-ray or magnetic resonance
imaging (MRI), may assist with diagnosis.
How is a suppressed immune system treated?
Individuals with a suppressed immune system will often be monitored for the development of infectious diseases, and they can be educated on infection prevention measures, including guidelines for self-isolation and personal protective equipment (PPE). An individual may also practice lifestyle behaviors that support their immune system, such as getting adequate sleep, exercising regularly, and eating a balanced diet with lots of fruits and vegetables. If infection occurs, antibiotics, like amoxicillin, or antivirals, like oseltamivir, may be prescribed depending on the specific bacterial or viral cause. Additional treatment for a suppressed immune system will vary by the underlying cause.
For autoimmune diseases, immunosuppressive medications are often prescribed.
HIV may be treated with antiretroviral therapy (ART), which aims to keep the virus from spreading throughout the body. HIV, as well as some cancers, may also be treated with immunomodulation therapy, medications that aim to improve and strengthen the immune response.
A person with splenic dysfunction may have a splenectomy, or surgery to remove their spleen. Although an individual can survive without a spleen, this will increase their risk of infection and sepsis. Because individuals without a spleen are at an increased risk of infections from encapsulated bacteria, vaccination against pneumococcus, meningococcus, and Haemophilus influenzae is advised after splenectomy.
For primary immune deficiency diseases, intravenous immunoglobulin treatments may be given to provide the individual with the specific antibodies they lack. Treatment can also include stem cell transplants or gene therapy, which promote the body’s intrinsic production of antibodies.
When the immunosuppression is caused by a medication, treatment usually focuses
on relieving the unwanted side effects. Such treatment can include medications to treat nausea (e.g., ondansetron) and pain-relieving medications (e.g., aspirin, ibuprofen).
If an infection occurs, the immunosuppressant’s dosage may be lowered, and depending on the infectious agent, antibiotics or antivirals may be prescribed. Less commonly, the immunosuppressive medication may be discontinued.
What are the most important facts to know about a suppressed immune system?
A suppressed immune system is weakened to the point that it leaves an individual vulnerable to infections. Immune system suppression can result from many causes, including diseases, medications, and lifestyle factors.
Most commonly, immune suppression happens due to an autoimmune disease,
such as lupus, rheumatoid arthritis, or type 1 diabetes.
The occurrence of frequent infections with severe symptoms is the primary sign
of a suppressed immune system. Immunosuppression is often diagnosed through a
medical examination and blood tests, typically including a complete blood count (CBC).
Most immunosuppression is treated by monitoring for infections, practicing lifestyle behaviors that boost the immune system, and taking medications to treat the associated symptoms and underlying cause. 10 Foods That May Weaken Your Immune System (healthline.com)
Humans’ slow metabolisms explain long life span, study says.
Though some individuals may not appreciate their slow metabolisms, a new study
suggests that humans and other primates – who burn 50% fewer calories each day
than other mammals – have such long lives because of their curiously slow metabolisms.
Publishing their results in the journal Proceedings of the National Academy of Sciences, the international team of scientists says burning fewer calories may also explain why primates grow up so slowly.
Though our pet dogs, cats or hamsters progress to adulthood much faster than we do, reproduce at a faster rate and sadly, die long before we will, humans and other primates – such as apes, monkeys and lemurs – have relatively long childhoods, do not reproduce as frequently and live longer lives.
The researchers note that the slow pace of the primate life has baffled biologists, as the underlying reasons for it were unclear. In order to better understand, the researchers examined 17 different primate species in zoos and sanctuaries, as well as in the wild, to assess their daily energy expenditure and determine whether their slow pace of life could be attributed to a slow metabolism.
Slow metabolic rate contributes to slow pace of aging
They employed a technique called “doubly labeled water,” which is non-invasive and tracks the body’s production of carbon dioxide. Using this technique, they were able to measure the calories that the primates burned for a duration of 10 days.
After establishing daily expenditure rates in primates, the team compared
them with the rates of other mammals.
According to Herman Pontzer, lead author of the study and anthropologist
at Hunter College in New York, the results surprised them:
“Humans, chimpanzees, baboons, and other primates expend only half the calories we’d expect for a mammal. To put that in perspective, a human – even someone with a very physically active lifestyle – would need to run a marathon each day just to approach the average daily energy expenditure of a mammal their size.”
Slow metabolism equals suppress immune system.
The researchers say that this reduction in primates’ metabolic rate explains their slow pace of life, and they add that energy expenditure can contribute to aging – as all organisms need energy to grow and reproduce.
“The environmental conditions favoring reduced energy expenditures may hold a key to understanding why primates, including humans, evolved this slower pace of life,” says David Raichlen, co-author of the study and anthropologist from the University of Arizona.
Though it seems logical that primates in captivity may not expend as many calories daily as those in the wild, the researchers found this is not the case. The captive primates expended just as many calories each day as those in the wild, which the team says may suggest that physical activity contributes less to total energy expenditure than we think.
Co-author Steve Ross, director of the Center for the Study and Conservation of Apes at Chicago’s Lincoln Park Zoo, says that the similarities in daily energy expenditures between wild and captive primates “demonstrates the depth of research potential” for zoo and sanctuary settings.
He suggests that these settings “represent an alternative to traditional laboratory-based investigations and emphasize the importance of studying animals in more naturalistic conditions.”
But the takeaway findings from the study – that daily energy expenditure may uncover how our bodies develop and age – have important implications for understanding health and life span in humans.
The researchers say unfolding the relationship between physical activity and daily energy expenditure may help us better understand metabolic diseases and obesity.
Herman Pontzer says they are already conducting more detailed research on the subject, adding:
“Humans live longer than other apes, and tend to carry more body fat. Understanding how human metabolism compares to our closest relatives will help us understand how our bodies evolved, and how to keep them healthy.”
Medical News Today recently reported on a study that suggested age-related weight gain may be due to brown fat failure. The researchers suggested as we age, our “good” brown fat is less efficient at burning calories.
Metabolism as a guiding force for immunity | Nature Cell Biology
BONUS: slow metabolism equals suppress immune system – Search (bing.com)
Tracing the relationship between metabolism and immune response
The delicate balance between our metabolism and our body’s immune response has critical implications for a range of chronic noncommunicable diseases, including obesity, diabetes, and cardiovascular disease. In a new review paper, published February 9, 2017, in the journal Nature, Gökhan S. Hotamisligil, J.S. Simmons Professor of Genetics and Metabolism and chair of the Department of Molecular Metabolism, traces the evolution of this relationship.
The way our bodies regulate and manage energy—our metabolism—and our body’s ability to defend itself against pathogens—the immune response—are closely linked because a strong immune response relies on energy, writes Hotamisligil. But an imbalance in this relationship can put us at risk for chronic metabolic diseases. Hotamisligil writes that there is now an opportunity to translate the increased knowledge about immunometabolism into interventions that one day may reduce the global burden
of those diseases.
Foods to enhance immune system – Bing video
Feeding your body certain foods may help keep your immune system strong.
If you’re looking for ways to prevent colds, the flu, and other infections, your first step should be a visit to your local grocery store. Plan your meals to include these 15 powerful immune system boosters. The idea of boosting your immunity is enticing, but the ability
to do so has proved elusive for several reasons. The immune system is precisely that —
a system, not a single entity.
Sleep Resets the Immune System – Search (bing.com)
Sleep provides essential support to the immune system. Getting sufficient hours of high-quality sleep enables a well-balanced immune defense that features strong innate and adaptive immunity, efficient response to vaccines, and less severe allergic reactions. In contrast, serious sleeping problems, including sleep … See more
To function well, it requires balance and harmony. There is still much that researchers don’t know about the intricacies and interconnectedness of the immune response.
For now, there are no scientifically proven direct links between lifestyle and
enhanced immune function.
But that doesn’t mean the effects of lifestyle on the immune system aren’t intriguing
and shouldn’t be studied. Researchers are exploring the effects of diet, exercise, age, psychological stress, and other factors on the immune response, both in animals and in humans. In the meantime, general healthy-living strategies make sense since they likely help immune function and they come with other proven health benefits.
GREAT VIDEOs How does sleep strengthen the immune system – Bing video
GREAT DIET FOR LYME DISEASE ![]() Calming Inflammation: Changing the Microbiome with the Specific Carbohydrate Diet with Pamela Ferro – YouTube
Calming Inflammation: Changing the Microbiome with the Specific Carbohydrate Diet with Pamela Ferro – YouTube
