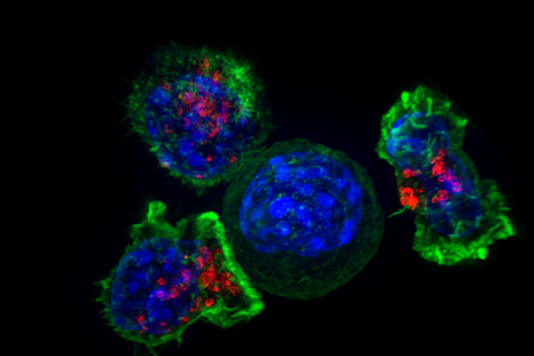
by releasing toxic chemicals (red), a move scientists have dubbed ‘the kiss of death.’
© NIH/Flickr Search Results for Brain Cancer | Cancer Quick Facts (solitarius.org)
Intratumoral IL-12 delivery empowers CAR-T cell immunotherapy
in a pre-clinical model of glioblastoma IL 12 Glioblastoma – Bing video
A novel immune-based, gene therapy approach is entering phase 2 trials (ClinicalTrials.gov Identifier: NCT04006119) for glioblastoma multiforme (GBM) after promising preliminary safety and efficacy data. Despite encouraging results in several tumor types such as melanoma, colorectal, and lung, immunotherapies have yet to show any significant benefit in patients with brain tumors. The new technique by Ziopharm hopes to reverse that trend.
“The brain is built to not be touched by our own immune system; it’s encased in the
dura and the blood brain barrier,” said Katy Peters, MD, PhD, neuro-oncologist at the Preston Robert Tisch Brain Tumor Center and associate professor of neurosurgery at
Duke University Medical Center, Durham, North Carolina. “In glioblastoma patients, white blood cells at diagnosis are sequestered in the bone marrow. This is our biggest hurdle — the immune cells are essentially unable to reach the tumor,” added Dr Peters.
There has been some recent evidence1,2 showing that immunotherapy treatment for melanoma or lung cancers can actually boost the immune response against metastatic disease in the central nervous system, but a general consensus remains that GBMs are fraught with an immunosuppressive environment.
Today’s top picks on the Haymarket Medical Network
Immunotherapy Works Well for Young Children With Peanut Allergy
Blood Type Associated With Immunotherapy Outcomes in RCC
Vision Abnormalities in Pediatric Brain Tumors Predictable With Structural Imaging
Experimental drug shown to ‘significantly’ slow progression of brain cancer (msn.com)
“[There are] several chemicals produced by GBM that make an immunosuppressive environment in general,” said Vyshak Venur, MD, medical oncologist at the Seattle Cancer Care Alliance and assistant professor at the University of Washington School of Medicine. “Glioblastoma also has a low mutational burden — unlike melanomas and lung cancers — which compounds this low response to immunotherapy,” he added.
GBM typically has a low tumor mutation burden and is considered immunologically “cold.” Several studies with PD-1 inhibitors, both alone, and in combination with drugs such as bevacizumab, have shown no significant benefit in patients. The Ziopharm approach uses an adenovirus vector encoding IL-12 — injected directly into the tumor —
in an attempt to boost immune recognition of the tumor.
“IL-12 can really be thought of as a master regulator of the immune system — it’s this molecule that [the] immune system uses as an alarm bell. If you have an infection, the
way that you recruit your immune system to a point of danger is via IL-12,” said Laurence Cooper, MD, PhD, CEO at Ziopharm.
Crucially, in contrast to most other gene-therapy approaches that use a viral vector, the production of IL-12 can then be “switched on” by the patient taking the small-molecule drug veledimex orally.
“This virus unpacks the IL-12 molecule, but it delivers it under the control of the switch
of a drug, so we can control the amount. If the immune response becomes too much, for example triggering a cytokine release syndrome (CRS), we can back off,” said Dr Cooper.
Researchers have been trying for years to utilize immunotherapy approaches:
against brain tumors with little success so far — so how unique is the Ziopharm approach?
“It is very innovative; what’s unique about this approach is that it is 2-pronged, where they are delivering the IL-12 to the tumor cavity itself and then using this activator of the IL-12 to control it,” said Dr Peters.
Updated results from an initial phase 1 study of the work using the IL-12 inducible therapy as a monotherapy (ClinicalTrials.gov Identifier: NCT02026271) and a dose-escalation sub study in combination with nivolumab (ClinicalTrials.gov Identifier: NCT03636477) were presented at the American Society of Clinical Oncology ASCO20 Virtual Scientific Program earlier this year.3
The data presented from 21 patients show a reasonable safety profile and evidence
of some preliminary immune effect, such as slightly increased cytotoxic T-cell counts in the peripheral blood.
“The study is very well done and concluding it’s safe is a good result for a phase 1 study. I’m not sure it’s reasonable to ask for significant efficacy data at this point, but that’s the reason that they are doing phase 2, which will give us a more robust idea of efficacy,”
said Dr Venur.
Today’s top picks on the Haymarket Medical Network
Sepiapterin Reduces Phenylalanine Levels in Patients With Phenylketonuria
Blood Type Associated With Immunotherapy Outcomes in RCC
Weight Fluctuations May Increase Cardiovascular Risk in Individuals With Type 2 Diabetes
“The first thing they show is they can do it safely. They are injecting a viral vector with
a gene activated along with a drug that can cause side effects. They were able to show
it’s safe and that some people see benefits,” said Dr Peters.
The presentation also featured 2 case reports of patients who
had partial responses on the combination therapy.
“One of the patients they showcase in the ASCO presentation had great response even up to week 36, which is very good for a patient with advanced GBM. These are early days, but it’s a promising approach,” said Dr Venur.
Despite a generally positive safety profile, there were still some concerns that two-thirds
of the treated patients displayed CRS, although all but one patient had grade 2, not grade 3, CRS.
“We are always worried about this effect [CRS] when we are stimulating a nonspecific immune response,” said Dr Venur. “This may be a barrier for this approach going forward, but we are really managing these side effects better, and we’ve learned a lot about these from [chimeric antigen receptor T-cell] treatments, for example,” he added.
Interestingly, the current situation with the COVID-19 pandemic may provide new information about treating CRS, which may be translational to managing the condition
in patients treated with chimeric antigen receptor T-cell (CAR-T) therapies.
“Given the situation with COVID-19 right now, where CRS is a significant concern, a lot
of new research is going into CRS — and we are going to learn more about it and how to suppress it. It’s an exciting paradigm,” said Dr Peters. “We are currently good at managing it and we are getting better,” she added.
Another hurdle that the therapy will have to navigate is dexamethasone.
Patients with glioblastoma are typically given dexamethasone to both control the symptoms of the tumor itself, such as brain swelling and edema, but also to control treatment side effects.
“Therapy itself can also cause swelling — radiation for example, radiation necrosis, swelling — and we use dexamethasone here, too,” said Dr Venur. “One big challenge
is that all of these patients are on dexamethasone as an immunosuppressive agent,”
who noted that this could affect the efficacy of the IL-12 therapy.
“I think it’s going to be a real problem to minimize steroids in these patients,” said
Dr Peters, who also noted that the authors of a 2019 paper showing preliminary results acknowledged this after observing an overall survival (OS) of 6.4 months compared with 16.7 months in patients who received more than 20 mg of steroids and for those who got less than 20 mg, respectively, on days 0-14 of the treatment.4
“They showed a big, big difference in OS in that paper. Steroids are a ubiquitous drug in our population — we’ve only got so many tools in our toolbox. It’s a necessary evil at the moment, and they will have to contend with this issue moving forward,” added Dr Peters.
“There is a huge drawback to steroids, as they handicap the immune response, but the need of this is being challenged. We are asking if patients really need all of these steroids. Many patients can go onto our clinical trial with low to negligible amounts of steroids,” said Dr Cooper, noting that Dr Chiocca, one of the lead clinical investigators of the trial,
is conducting investigations on this specific topic.
The aforementioned phase 2 trial expects to recruit 30 to 40 patients with recurrent or progressive GBM. Patients will receive an intratumoral injection of the IL-12 gene therapy, daily oral veledimex, and the trial will use infusions of the PD-1 antibody cemiplimab-rwlc every 3 weeks.
“We expect to have data from these patients within this year and next,” said Dr Cooper. “With the monotherapy, we have a median OS of 16 months, so we already see improvement. In the phase 2 trial, we will ask the question of whether we can
get past 16 months of OS.”
The gene therapy is also being trialed in children with diffuse intrinsic pontine glioma (DIPG), which is almost universally fatal, and where there is a huge unmet need for new treatment approaches. A phase 1/2 trial (ClinicalTrials.org Identifier: NCT03330197) of the human IL-12 vector (transcriptionally regulated by the oral activator veledimex) as a monotherapy has begun, with the first patient recently treated at Lurie Children’s Hospital in Chicago. The trial hopes to recruit up to 12 patients in total to evaluate the safety and tolerability of the therapy in pediatric DIPG patients.
References
Queirolo P, Spagnolo F, Ascierto PA, et al. Efficacy and safety of ipilimumab in patients with advanced melanoma and brain metastases. J Neurooncol. 2014; 118(1):109-116. doi:10.1007/s11060-014-1400-y
Goldberg SA, Schalper KA, Gettinger SN, et al. Pembrolizumab for management of patients with NSCLC and brain metastases: long-term results and biomarker analysis from a non-randomised, open-label, phase 2 trial. Lancet Oncol. 2020;21(5):655-663. doi: 10.1016/S1470-2045(20)30111-X
Chiocca EA, Lukas RV, Chen CC, et al. Evaluation of controlled IL-12 in combination with a PD-1 inhibitor in subjects with recurrent glioblastoma. J Clin Oncol. 2020;38(15_suppl):2510-2510. doi:10.1200/JCO.2019.37.15_suppl.2020
Chiocca EA, Yu JS, Lukas RV, et al. Regulatable interleukin-12 gene therapy in patients with recurrent high-grade glioma: Results of a phase 1 trial. Sci Transl Med. 2019;11(505):eaaw5680. doi:10.1126/scitranslmed.aaw5680
IL-12B & IL-12A Molecule Background
Interleukin 12 (IL12) is also known as p70, and is an interleukin that is naturally produced by dendritic cells, macrophages and human B-lymphoblastoid cells (NC-37) in response to antigenic stimulation.IL12 is a heterodimeric cytokine, containing IL-12A (p35) and IL-12B (p40). IL-12 is involved in the differentiation of naive T cells into Th1 cells.
It is known as a T cell-stimulating factor, which can stimulate the growth and function
of T cells. It stimulates the production of IFN-γ and TNF-α from T cells and NK cells and reduces IL-4 mediated suppression of IFN-γ. IL-12 plays an important role in the activities of natural killer cells and T lymphocytes. IL-12 also has anti-angiogenic activity, which means it can block the formation of new blood vessels.
IL-12B & IL-12A Protein – ACROBiosystems
Intratumoral IL-12 delivery empowers CAR-T cell immunotherapy in
a pre-clinical model of glioblastoma – PubMed (nih.gov)
Integrative Oncologists Providing Holistic Cancer Treatment Options for Early,
Late-Stage, and Metastatic Cancer | Envita Medical Centers
‘Masked’ cancer drug stealthily trains immune system to kill tumors while sparing
healthy tissues, reducing treatment side effects (msn.com)
Report links toxic substance to cancer deaths in at least six baseball players:
‘What happened to exercising caution?’ (msn.com)
An investigation showing a possible link between brain cancer and artificial turf strengthened a key argument among champions for natural grass — that nature does it better. The Philadelphia Inquirer reported on examinations into the deaths of six former Philadelphia Phillies, who spent much of their baseball careers playing on fake turf at Veterans Stadium, which was open from 1971 to 2003.
These players died in their 40s and 50s from a rare form of brain cancer, glioblastoma.
They played atop an artificial field made in part with so-called forever chemicals that are linked to cancer. While experts can’t say for certain that the field caused the disease, the reports are leading to more scrutiny of fake grass around the country.
“We don’t know what those chemicals are doing to us — what happened to exercising caution when we’re talking about human health?” Kyla Bennett, a former scientist for
the Environmental Protection Agency, said to the Guardian, which also reported on the deaths. Bennett now works for Public Employees for Environmental Responsibility.
What is artificial turf?
Artificial turf, also known as synthetic turf or fake grass, is exactly what it sounds like —
a surface made from synthetic materials, primarily plastic, that is designed to mimic the look and feel of real grass.
Modern forms of artificial lawns include green synthetic grass over crumb rubber,
which is often made from old tires, according to the Center for Environmental Health.
Veterans Stadium had a form of artificial turf that was popular for fields built in the 70s
and 1980s, the Guardian reports, noting that all artificial turf contains forever chemicals.
Because those chemicals break down very slowly.
Why are the fields still a concern?
Faux-grass fields remain popular in the U.S., with about 1,200 being added each year to the existing 12,000, according to the Guardian. Athletes from school age to professionals play on them. Forever chemicals, also called PFAS, have possible links to increased risks for cancers throughout the body, the American Cancer Society reports.
The health impact of the more than 9,000 PFAS so far discovered is still being studied.
Experts, including Bennett, don’t understand why fields with forever chemicals are still being made. “Is artificial turf easier? Yeah, you don’t have to mow it, but that doesn’t
mean it’s right to use it,” she told the Guardian.
The Brain Cancer That Keeps Killing Baseball Players (nytimes.com)
In 2013, when Daulton learned he had glioblastoma, The Philadelphia Inquirer did an analysis of 533 players who also wore a Phillies uniform during the 33 seasons the team played at Veterans Stadium. The brain cancers of Daulton, McGraw, Vukovich and Oates appeared to represent an occurrence that was about three times the rate of the general male population, the analysis concluded. But the study had limitations related to adjusting for age and yearly cancer rates.
Professor Rebbeck, the Harvard epidemiologist, was then at the University of Pennsylvania, and he assisted in the study. He told The Inquirer that the seemingly elevated risk to baseball players could have resulted from chance.
In an interview after Daulton’s death, Professor Rebbeck said scientists still did not know much more. “It’s either just random chance bad luck or there is something there, but we just don’t have the science to pick it out yet,” he said.
The baseball deaths fit within established patterns in the general population: Glioblastoma is more common among men than women, and the risk increases with age. The scrutinized baseball deaths have occurred within the highest-risk age range of 45 to 70, according to the American Association of Neurological Surgeons. An estimated 12,390 new cases of the cancer were expected this year, according to the American Brain Tumor Association.
Researchers also note that while the players’ cancers have been identified as glioblastomas in news media accounts, all may not, in fact, have been identical tumors. Many other variables make it difficult to make a connection between baseball and brain cancer.
Among the former Phillies who died, not all played together at Veterans Stadium or remained with the team for the same length of time. The Philadelphia Eagles played and often practiced in the stadium, on the same artificial surface, but the N.F.L. team has reported no unusual occurrence of brain cancer.
This in memory of Tug McGraw, along with five other former Phillies players—
David West, John Vukovich, Johnny Oates, Ken Brett, and Darren Daulton—were
all diagnosed with, and later passed away from, glioblastoma.
The research continues.
Most scientists use words like “link” and “suggest” to describe the relationship
between forever chemicals, artificial fields, and cancer. “There is no way to now say,
‘If these chemicals are there, they are causing the tumors,’” Dr. Henry Friedman,
a neuro-oncologist at Duke University, told the Guardian.
He treated two of the Phillies. For their part, artificial turf makers told the Guardian
their products “meet and exceed” health standards and that they benefit communities.
The Mystery 0f Cancer Cluster @Erin Brockovich.
Cancer Cluster in Clyde Ohio – Search (bing.com)
What can I do to help?
For natural grass advocates like Bennett, the information cited by the Philadelphia Inquirer, the Guardian, and other news outlets is reason enough to ban artificial turf.
Organizations like Turfgrass Producers International are a great resource to learn about the health benefits of natural grass — for the body and the planet. A little research can equip lawn lovers with solid facts to take to school boards and other officials who may consider installing an artificial field. ‼Re. THE SOUTH SLAVS: Sofia, Bulgaria’s capital,
is one of the oldest cities in the world.




/BTW, the great majority of those living in Slavic countries ….
(Bulgarian, Russian, Polish, etc.) oppose the Democrats,
Communism, Globalism, and Islam./ like Americans

– — Yandex Images
