© Provided by New York Post
Obesity is known to increase the risk of cancer — but which kinds of cancer?
New research has found that the answer differs between men and women,
and depends in part on where fat is located on the body.
“Doctors and scientists are aware that obesity increases cancer risk, but this connection
is less well known to members of the public,” study author Mathias Rask-Andersen,
a researcher at Uppsala University in Sweden, said in a news release.
To investigate the links between cancer and obesity among men and women, Rask-Andersen and other researchers turned to the UK Biobank, a biomedical database with genetic and health information from more than half a million participants across the UK.
The massive database also includes information on the distribution of fat in participants’ bodies and their cancer history, if any. “An important aspect of obesity-associated disease risk is the distribution of fat in different compartments of the body,” said co-author
Asa Johansson, also of Uppsala University.
“Fat stored in the abdomen is considered more pathogenic [disease-causing] compared
to subcutaneous [below the skin] fat. In addition, the amount of fat stored in different compartments, as well as the rates of most cancers, is known to differ between females
and males,” Johansson said.
Among their findings, the research team discovered that all cancer types except brain, cervical and testicular cancers are associated with obesity.
Men with obesity were found to be at higher risk for breast cancer, hepatocellular carcinoma and renal cell carcinoma. For women with obesity, the highest risks were associated with gallbladder cancer, endometrial cancer and esophageal adenocarcinoma.
Obesity is a well-known risk factor for cancer — but which types, and in whom?
A new study defines how various forms of fat lead to different cancers in men & women.
And in terms of fat distribution versus fat accumulation, there were different effects between men and women for colorectal, esophageal and liver cancer.
For men, body fat accumulation was linked to a high risk for hepatocellular carcinoma,
but the same link was not seen among women. And unlike men, women with a larger proportion of fat stored in the abdomen had a higher risk of esophageal squamous cell carcinoma.
“We were surprised to see that there appeared to be a difference in the effect of obesity
on cancer risk, not only between males and females, but also between post- and pre-menopausal females,” Johansson said.
“Most remarkable, obesity is only a risk factor for breast cancer after menopause, probably due to the change in estrogen production in association with menopause,” she added.
The authors noted that rising rates of obesity make their research especially timely.
“Given the rapidly increasing rates of obesity globally, obesity is now the fastest-growing risk factor for overall cancer risk,” Rask-Andersen said. “Measures to prevent and reduce the occurrence of obesity and being overweight are therefore highly motivated.
“However, it is important to consider that reducing weight does not eliminate the risk
of cancer. There are still many individual risk factors that play a much larger impact on specific types of cancer, such as smoking for lung cancer and exposure to sun for skin cancer,” he added. Obesity and Cancer Locations – Bing video
43% of the worldwide population has an obesity-associated gene (FTO), making it the most common gene that can cause obesity.
Whilst Samoa has the highest rates of obesity in men, with a total of 60.8% of its male population. Tonga has 82.8% of their female population living with obesity.
According to the CDC, the average annual medical cost for handling obesity and obesity-related comorbidities was $147 billion in 2008. Image: en.wikipedia.org. Data: Wikipedia · cerbariatrics.com · loudcloudhealth.com · obesityreporter.com
Wikipedia text under CC-BY-SA license
 Healthy Living Tips
Healthy Living TipsCommon Health Risks of Obesity
Obesity is often associated with physical strain on the body, contributing to disease and other conditions. It can also have an adverse impact on social and emotional well-being, and it’s commonly linked to deep feelings of sadness, self-blame and depression.
These symptoms should not be ignored. Doctors and psychiatrists should work
together to address your total health.
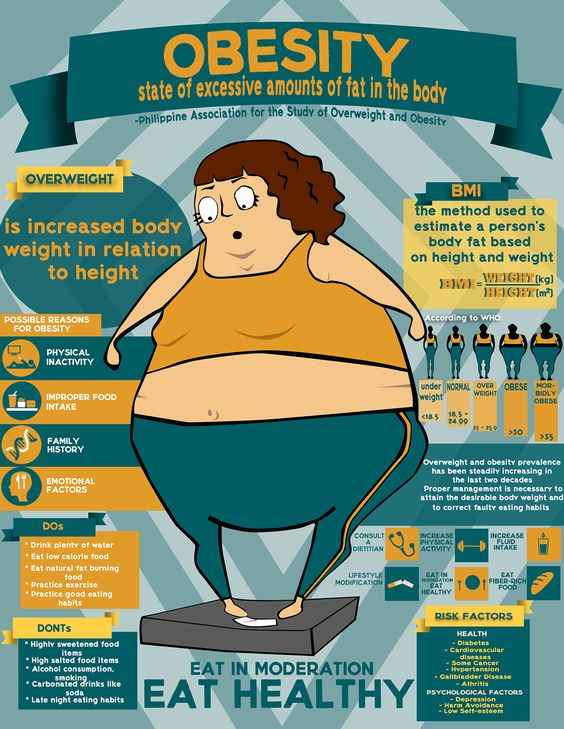
If you struggle with weight, use a BMI calculator to estimate your potential link
to disease risk. The Body Mass Index, or BMI, provides you with the healthy weight
range for your height. While it doesn’t take into account age, gender or activity level,
it is the method most commonly used to indicate the presence of body weight concerns.
Talk to your doctor to find out if your weight is affecting your health and consider the
help of a nutritionist or dietician.


Take control of your weight.
Call an HHC hospital or healthcare center in your area to ask about weight management programs and support groups. It’s all about creating an understanding that obesity can impact the:
MIND
Obesity goes deep. Assumptions and biases that exist around weight can have a real and cumulative impact on mental health and morale. People may internalize this weight bias and blame themselves, leading to depression, anxiety and low self-esteem.


BODY
Weight management is not just about willpower. Many factors are also at play within
our bodies, including genetics and biology, which can impact how we gain, lose and regain weight. These factors make living with obesity a unique journey for everyone and also play a role in physical health, with links to at least 60 other health conditions.
SOCIETY
Weight bias still exists. It leaves people feeling judged in society. Weight bias can be present in most areas of our life, including at work, in the doctor’s office, on the shows we watch, among friends and family, and more. In addition, factors like socioeconomics and cultural influence can sometimes contribute to further biases.

Spirituality
Using the Nurses’ Health Study II cohort, follow-up occurred from 2001 to 2015, with up to 35,547 participants assessed for the religious or spiritual coping and religious service attendance analyses. Cox regression and generalized estimating equations evaluated associations with obesity and weight change, respectively. Religious or spiritual coping and religious service attendance had little evidence of an association with obesity.
Compared with not using religious or spiritual coping at all, the fully adjusted hazard ratios (HRs) were minimally different across categories: a little bit (HR = 1.05, 95% CI: 0.92–1.18), a medium amount (HR = 1.09, 95% CI: 0.96–1.24), and a lot (HR = 1.10; 95% CI: 0.96–1.25) (Ptrend = 0.17).
Compared with participants who never or almost never attend religious meetings or services, there was little evidence of an association between those attending less than once/month (HR = 1.08, 95% CI: 0.97–1.10), 1–3 times/month (HR = 1.01, 95% CI: 0.90–1.13), once/week (HR = 0.92, 95% CI: 0.83–1.02), and more than once/week (HR = 0.94, 95% CI: 0.82–1.07) (Ptrend = 0.06).
Findings were similar for weight change.
There was no significant association between religious or spiritual coping, religious service attendance, obesity, and weight change. While religion and spirituality are prominent in American society, they are not important psychosocial factors influencing body weight in this sample.
New scientific findings reveal neuroinflammation as key factor in alcohol-induced pain.
12 Foods People Hated As Kids Then Realized Their Parents Just Didn’t Cook It Right.
15 Things You Do That Signals To Everyone Around You That You’re Insecure (msn.com)
Home Depot worker claims she’s ‘too pretty’ to work at the store (msn.com)
The Biggest Food Fads of the Past 50 Years (msn.com)
By shattering these misconceptions, real change will come in understanding that
biology and genetics play a role alongside diet and other factors. Then, it’s about putting
a spotlight on the need we have for better care and compassion from everyone–family, friends, coworkers, strangers and even doctors.
It only takes a spark to light a fire.
Let’s ignite a chain reaction that ends shame and shatters the misconceptions.
It’s bigger than numbers on a scale. It’s bigger than diet and exercise.
It’s bigger than lifestyle choices.
Together, as a movement, community and society, we can create real change.
Join Us on Instagram: It’s Bigger Than Me (@itsbiggerthan) • Instagram photos & videos
and also Make a Plan with Your HCP to Lose Weight & Maintain it | Truth About Weight®
