What is Auto Immune Disease – Bing video
In such cases, the body often attacks and damages its own tissues. Immune deficiency diseases reduce the body’s ability to battle invaders, resulting in vulnerability to infections.
In response to an unfamiliar trigger, the immune system may start producing antibodies that instead of working against infections, start attacking the body’s own tissues.
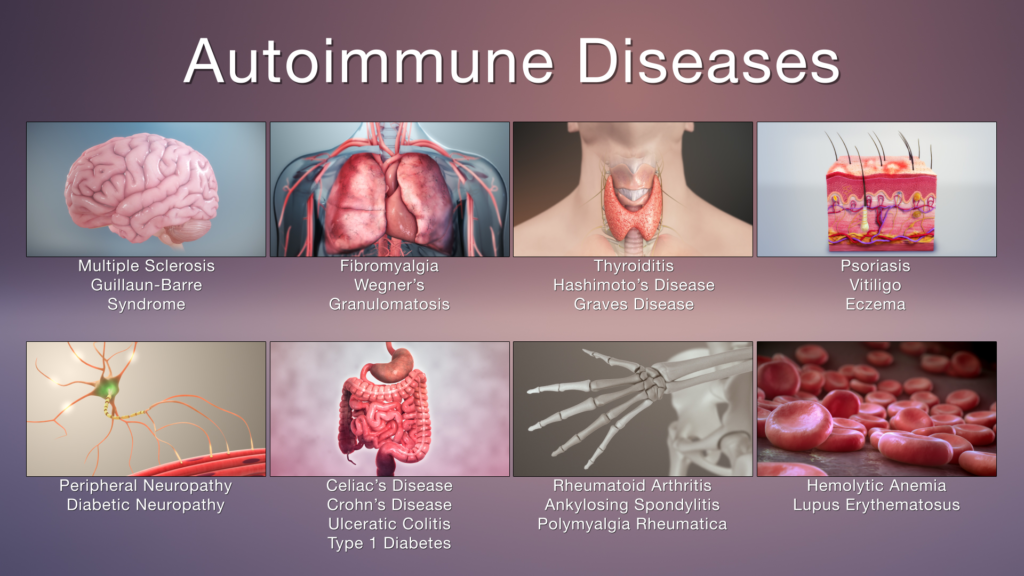
There are over 80 various autoimmune diseases.
Here are few of the most common ones:
Rheumatoid arthritis (RA)
Systemic lupus erythematosus (SLE)
Inflammatory bowel disease
Multiple sclerosis
Type 1 diabetes
Celiac disease
Myasthenia gravis
Psoriasis
Graves’ disease
and more.
Autoimmune disease symptoms
The early symptoms of various autoimmune diseases
are quite similar, such as:
Fatigue
Ache in muscles
Swelling
Low-grade fever
Redness
Skin rashes
Numbness and tingling in the hands and feet
Loss of hair
Trouble in concentrating
Individual diseases could have their own unique symptoms as well.
Treatments can’t usually cure autoimmune diseases, however, they can help control the overactive immune response and decrease inflammation or reduce pain. Some of the drugs used to treat these conditions include:Nonsteroidal anti-inflammatory drugs (NSAIDs)
Immune-suppressing drugs
Some treatments are also available to alleviate symptoms such as pain,
inflammation, skin rashes and fatigue.
One should consider consuming a well-balanced diet and performing regular exercise may also aid you feel better.
Over 80 various autoimmune diseases exist. Quite often their symptoms overlap, making them difficult to diagnose.
Autoimmune diseases are more common in women, and they usually run in families.
Disclaimer: The information in no way constitutes or should be construed as medical advice. Nor is the above article an endorsement of any research findings discussed in the article an endorsement for any of the source publications.Sources-
https://www.webmd.com/a-to-z-guides/autoimmune-diseases
https://www.healthline.com/health/autoimmune-disorders#symptoms
Diet in Autoimmune Disease
Make your Diet Work for You
By Elaine Moore
Certain foods known as immunity boosters:
aid the healing process in people with autoimmune disorders.
Autoimmune Disease Diet: 6 Foods to Eat and 3 to Avoid (food revolution.org)
Defining a Good Diet

A good diet has long been considered the basis of good health.
The simple term good diet refers to a diet that provides the countless nutrients present in whole foods that are essential for life and provided in a well-balanced diet. In addition, these foods should be free of chemical contaminants and contain an abundant supply of vitamins and minerals. A good diet contains an assortment of foods rich in vitamins A, B complex, C and E; foods with high mineral content, particularly zinc, selenium, calcium and magnesium; foods rich in omega-3 and omega-6 fatty acids such as oily fish, seeds and nuts; adequate protein from lean meats and grain; fiber from grains, fruit and vegetables.
To prevent allergies the diet should be varied and the same foods shouldn’t be eaten on a daily basis. Vitamin C found in many fruits and vegetables is needed by all of the immune system’s cells to carry out their functions. Vitamin A found in liver, dairy products, oily fish and plant foods is essential for the thymus gland, an immune system organ necessary for the proper maturation of immune system cells.
B vitamins and calcium are needed for white blood cells known as phagocytes and for proper skeletal muscle and nervous system function. Vitamin E, zinc, and selenium are powerful antioxidants needed to reduce oxidative stress and for antibody production.
All immune system cells require protein for their continued production.
Protein sources are also needed for the production of amino acids and antibodies.
‘I’m a Gastro, and Eating More of These Fermented Foods Can Boost Your Sleep—
In Addition to Your Digestion’ (msn.com)
Immune System Effects
A good diet can strengthen, not stimulate, the immune system and enable all of the body’s organs to carry on with their intended functions. On the other hand, a bad diet contains food ladled with pesticides, chemical preservatives, artificial sweeteners, and stabilizers that are detrimental to our health. For instance, the unnatural composition of iodized food products, while preventing iodine deficiency in certain regions, has been found to trigger autoimmune thyroid disease worldwide. And certain molecules in genetically engineered products are recognized as foreign by our immune systems, and in turn, our immune systems are stimulated and weakened, which promotes autoimmune disease development.
Chemical Toxins
Chemicals such as chlorine and fluoride added to our water supplies also cripple the immune system, as do antibiotics added to the grains fed to cattle and poultry. It’s not surprising that many people with penicillin allergies develop hives or symptoms of anaphylaxis after eating poultry or beef.
For those of us with autoimmune diseases, maintaining a good diet involves avoiding processed foods, buying free range or organic meat products, and adding foods known to be top immunity boosters to our diets.
An efficient functioning immune system is essential for good health and for the prevention and healing of autoimmune diseases. An efficient immune system also protects us from infection and cancerous growths and helps temper the allergic response. Signs of a poorly functioning immune system include autoimmune diseases, digestive problems, fatigue, joint pain, muscle weakness, food intolerances, allergies, and poor skin.
Top Immunity Boosters
Different foods differ not only in taste and appearance but also in their nutrient content. The top immunity boosters listed in this article include foods with the proven ability to improve immune system health. In some cases, specific nutrients can only be found in a scattering of different foods, foods considered essential for immune health.
While dietary supplements are another important component of immune system health, many nutrients can’t be adequately extracted from food sources and can only be obtained from eating whole foods.
And since many nutrients are only found in foods of a certain color, dietary experts recommend choosing foods from a broad spectrum of colors for optimal health.
The top 10 immune system boosters, which supply the highest levels of these nutrients, include beets, shiitake mushrooms, avocado, curly kale, grapefruit, blueberry, Brazil nuts, soybeans, green tea and garlic.
Other top immune boosters include sweet potatoes, carrots, onions, garlic, yams, red bell peppers, tomatoes, rhubarb, pumpkin, chili peppers, avocadoes, cruciferous vegetables, watercress, nettle, spinach, Belgian endive, globe artichokes, arugula, kiwi, pineapple, papayas, mangoes, guava, cantaloupe, passion fruits, citrus fruits, bananas, grapes, berries, rosehips, hazelnuts, apples, endive, walnuts, cashews, almonds, pistachio nuts, sunflower and pumpkin seeds, safflower oil, evening primrose oil, sesame seed and oil, aduki beans, oats, wheat germ, quinona, bulgur, rice, corn, kidney beans, lima beans, green beans, lentils, snow peas, turkey, guinea fowl, pheasant, duck, chicken, fresh tuna, salmon, anchovy, mackerel, shrimp, yogurt, peppermint, chamomile, rosemary, ginger and turmeric. These foods all contain an abundance of nutrients with antioxidant,
immune restoring or anti-inflammatory properties.

© 3 Sep 2006 Copyrighted by Elaine Moore
Resource: The Top 100 Immunity Boosters: 100 Recipes to Keep Your Immune System Fighting Fit: Haigh, Charlotte: 9781844831111: Amazon.com: Books London: Duncan-Baird, 2005.
AIP (Autoimmune Protocol) Diet: A Beginner’s Guide
How to Tackle the Relationship between Autoimmune Diseases and Diet: Well Begun Is Half-Done – PMC (nih.gov)
An Autoimmune Protocol (AIP) diet plan can be similar to the paleo diet but is usually stricter. It primarily involves eliminating certain foods that may cause inflammation and reintroducing them gradually once symptoms improve.
The AIP diet aims to reduce inflammation, pain, and other symptoms caused by autoimmune diseases, such as lupus, inflammatory bowel disease (IBD), celiac disease, and rheumatoid arthritis (1Trusted Source).
Many people who have followed the AIP diet report improvements in how they feel, as well as reductions in common symptoms of autoimmune disorders, such as fatigue and gut or joint pain. Yet, while research on this diet is promising, it’s also limited.
This article offers a comprehensive overview of the AIP diet, including the science behind it, as well as what is currently known about its ability to reduce symptoms of autoimmune disorders.
What is the Autoimmune Protocol Diet?
A healthy immune system is designed to produce antibodies that attack foreign or harmful cells in your body.
However, in people with autoimmune disorders, the immune system tends to produce antibodies that, rather than fight infections, attack healthy cells and tissues.
This can result in a range of symptoms, including joint pain, fatigue, abdominal pain, diarrhea, brain fog, and tissue and nerve damage.
A few examples of autoimmune disorders include rheumatoid arthritis, lupus, IBD, type 1 diabetes, and psoriasis.
Autoimmune diseases are thought to be caused by a variety of factors, including genetic propensity, infection, stress, inflammation, and medication use.
Also, some research suggests that, in susceptible individuals, damage to the gut barrier can lead to increased intestinal permeability, also known as “leaky gut,” which may trigger the development of certain autoimmune diseases (2Trusted Source).
Certain foods are believed to possibly increase the gut’s permeability, thereby increasing your likelihood of leaky gut.
The AIP diet focuses on eliminating these foods and replacing them with health-promoting, nutrient-dense foods that are thought to help heal the gut, and ultimately, reduce inflammation and symptoms of autoimmune diseases (3Trusted Source).
It also removes certain ingredients like gluten, which may cause abnormal immune responses in susceptible individuals (4Trusted Source, 5Trusted Source).
While experts believe that a leaky gut may be a plausible explanation for the inflammation experienced by people with autoimmune disorders, they warn that the current research makes it impossible to confirm a cause-and-effect relationship between the two (2Trusted Source).
Therefore, more research is needed before strong conclusions can be made.
SUMMARY The Autoimmune Protocol (AIP) diet is purported to reduce inflammation, pain, and other symptoms experienced by people with autoimmune disorders by healing their leaky gut and removing potentially problematic ingredients from their diet.
How does it work?
The AIP diet resembles the paleo diet, both in the types of foods allowed and avoided,
as well as in the phases that comprise it. Due to their similarities, many consider the AIP diet an extension of the paleo diet — though AIP may be seen as a stricter version of it.
The AIP diet consists of two main phases.
The elimination phase
The first phase is an elimination phase that involves the removal of foods and medications believed to cause gut inflammation, imbalances between levels of good and bad bacteria in the gut, or an immune response (1Trusted Source, 3Trusted Source).
During this phase, foods like grains and gluten, legumes, nuts, seeds,
nightshade vegetables, eggs, and dairy are completely avoided.
Tobacco, alcohol, coffee, oils, food additives, refined and processed sugars, and certain medications, such as non-steroidal anti-inflammatory drugs (NSAIDs) should also be avoided (1Trusted Source).
Examples of NSAIDs include ibuprofen, naproxen, diclofenac, and high dose aspirin.
On the other hand, this phase encourages the consumption of fresh, nutrient-dense foods, minimally processed meat, fermented foods, and bone broth. It also emphasizes the improvement of lifestyle factors, such as stress, sleep, and physical activity (1Trusted Source).
The length of the elimination phase of the diet varies, as it’s typically maintained until a person feels a noticeable reduction in symptoms. On average, most people maintain this phase for 30–90 days, but some may notice improvements as early as within the first 3 weeks (1Trusted Source, 6Trusted Source).
Home – A Gutsy Girl®
The reintroduction phase
Once a measurable improvement in symptoms and overall well-being occurs, the reintroduction phase can begin. During this phase, the avoided foods are gradually reintroduced into the diet, one at a time, based on the person’s tolerance.
The goal of this phase is to identify which foods contribute to a person’s symptoms and reintroduce all foods that don’t cause any symptoms while continuing to avoid those that do. This allows for the widest variety a person can tolerate. Recipes – A Gutsy Girl®
During this phase, foods should be reintroduced one at a time, allowing for a period
of 5–7 days before reintroducing a different food. This allows a person enough time to notice if any of their symptoms reappear before continuing the reintroduction process (1Trusted Source).
Foods that are well tolerated can be added back into the diet, while those that trigger symptoms should continue to be avoided. Keep in mind that your food tolerance may change over time.
As such, you may want to repeat the reintroduction test for foods that initially failed the test every once in a while.
Step-by-step reintroduction protocol
Here’s a step-by-step approach to reintroducing foods that were avoided during the elimination phase of the AIP diet.
Step 1. Choose one food to reintroduce. Plan to consume this food a few times per day on the testing day, then avoid it completely for 5–6 days.
Step 2. Eat a small amount, such as 1 teaspoon of the food, and wait 15 minutes to see if you have a reaction.
Step 3. If you experience any symptoms, end the test and avoid this food. If you have no symptoms, eat a slightly larger portion, such as 1 1/2 tablespoons, of the same food and monitor how you feel for 2–3 hours.
Step 4. If you experience any symptoms over this period, end the test and avoid this food. If no symptoms occur, eat a normal portion of the same food and avoid it for 5–6 days without reintroducing any other foods.
Step 5. If you experience no symptoms for 5–6 days, you may reincorporate the tested food into your diet, and repeat this 5-step reintroduction process with a new food.
It’s best to avoid reintroducing foods under circumstances that tend to increase inflammation and make it difficult to interpret results. These include during an infection, following a poor night’s sleep, when feeling unusually stressed, or following a strenuous workout.
Additionally, it’s sometimes recommended to reintroduce foods in a particular order.
For example, when reintroducing dairy, choose dairy products with the lowest lactose concentration to reintroduce first, such as ghee or fermented dairy products.
Supplements:
Low-dose naltrexone (LDN):
A promising treatment in immune-related diseases and cancer therapy.
Naltrexone, a non-selective antagonist of opioid receptors, is mainly used as rehabilitation therapy for discharged opiate addicts to eliminate addiction in order to maintain a normal life and prevent or reduce relapse. In recent years, there have been some novel and significant findings on the off-label usage of naltrexone. Within a specific dosage window, LDN can act as an immunomodulator in multiple autoimmune diseases and malignant tumors as well as alleviate the symptoms of some mental disorders. The results of increasing studies indicate that LDN exerts its immunoregulatory activity by binding to opioid receptors in or on immune cells and tumor cells. These new discoveries indicate that LDN may become a promising immunomodulatory agent in the therapy for cancer and many immune-related diseases. In this article, we review the pharmacological functions and mechanisms of LDN as well as its clinical therapeutic potential as revealed by our team and other researchers.
LDN AND AUTOIMMUNE DISEASE – Bing video
Elaine Moore Graves’ Disease and Autoimmune Disease Education > Articles >
Low Dose Naltrexone Articles > Benefits of Low Dose Naltrexone (elaine-moore.com)
Hydroxychloroquine: initially used as an antimalarial, is used as an immunomodulatory and anti-inflammatory agent for the management of autoimmune and rheumatic diseases such as systemic lupus erythematosus. Lately, there has been interest in its potential efficacy against severe acute respiratory syndrome coronavirus 2, with several speculated mechanisms. The purpose of this review is to elaborate on the mechanisms surrounding hydroxychloroquine. The review is an in-depth analysis of the antimalarial, immunomodulatory, and antiviral mechanisms of hydroxychloroquine, with detailed and novel pictorial explanations. The mechanisms of hydroxychloroquine are related to potential cardiotoxic manifestations and demonstrate potential adverse effects when used for coronavirus disease 2019 (COVID-19). Finally, current literature associated with hydroxychloroquine and COVID-19 has been analyzed to interrelate the mechanisms, adverse effects, and use of hydroxychloroquine in the current pandemic. Currently, there is insufficient evidence about the efficacy and safety of hydroxychloroquine in COVID-19.
Hydroxychloroquine and AutoImmune Disease – Bing video
*MUST WATCH: Discovery Health – Celiac Disease. – YouTube
Eamon Murphy celiac disease – Search (bing.com) | Eamon Murphy?
Celiac.com 03/11/2022 – As many of you already know, celiac disease can be associated with quite a few other autoimmune diseases such as lupus, fibromyalgia, Crohn’s, Sjogren’s, multiple sclerosis, diabetes, etc.
In addition, celiac disease can also be connected with a few hormonal issues such as thyroid disease (specifically Hashimoto’s), adrenal fatigue, and high/low levels of estrogen.
For those with celiac disease and hormonal issues, some of the symptoms you can experience include hot flashes, insomnia, headaches, weight gain or loss, fatigue, muscle spasms, heavy menstrual cycles, heart rate changes, and much more.
There are many ways you can treat hormone imbalances, but many people prefer
to first try more natural methods, in the hope of avoiding pharmaceutical medications.
For those in this group, nutrition can be an excellent way to help stabilize your body’s estrogen levels and feel better fast. Foods to eat include pistachios, artichokes, cruciferous vegetables (broccoli, Brussels sprouts, kale, and cauliflower), chia and hemp seeds.
Simply by incorporating these nuts, seeds, and vegetables into your daily lifestyle,
you’ll begin to feel more energetic and have less pain.
Even if you don’t happen to be living an allergen-friendly life, these foods can definitely be beneficial for hormonal regulation. For those with celiac disease, eating gluten-free foods can help reduce the intensity of your thyroid and adrenal fatigue symptoms.
There are even certain herbs that can be beneficial for your hormone levels, and picking the right ones, of course, will depend on your body’s individual needs. From maca, yarrow, red raspberry, ashwagandha, chase tree, black cohosh, mother wart, mugwort, shepherd’s purse, stinging nettle, to burdock. Choosing the right one may help decrease fatigue, lessen menstrual pain, reduce hot flashes, and ease headaches. Be sure to read up on the known side-effects of any of these herbs before taking them, as they may interfere with other conditions you may have, for example ashwagandha can increase your blood pressure.
BONUS:
Reversing autism naturally – Bing video
Reversing autism with diet – Bing video
Reversing autism with nutrition – Bing video
